Managing type 1 diabetes is tricky business.
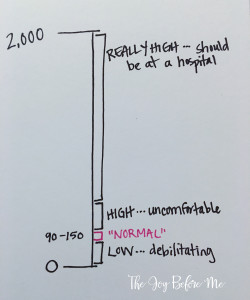
Together with our medical team, we have a target range for Mackenna’s blood glucose (BG) set at 90-150. If her BG goes lower than that, she can experience symptoms of hypoglycemia like dizziness, blurry vision, weakness/fatigue, difficulty focusing. In order to combat a low BG, she needs to consume some fast-acting sugar: juice, applesauce, raisins, glucose tabs, skittles. If left untreated, her BG could continue to drop which could lead to seizures, unconsciousness or worse. A low BG can get quite dangerous pretty quickly and needs immediate attention.
On the flip side, if Mackenna’s BG climbs above her target range, she can experience symptoms of hyperglycemia. A high BG makes her feel crummy. She is thirsty, gets a headache, and feels nauseous. We combat a high BG with insulin, just like a pancreas would. If her BG remained high for too long, she may develop ketones in her blood and land herself in the hospital. Maintaining high BG levels over long periods of time has negative long term effects on a person’s body. This truth is never far from my mind as I know she’s got a lot of living left to do and I want her to have the best future possible!
The problem with managing type 1 is that in the diabetes world, 1 + 1 does not always equal 2. We can do the exact same activities at the exact same times, eat the same amounts of the same exact things on two different days and get completely different BG numbers. It’s seriously maddening! There are hundreds of variables that can affect blood glucose numbers. Here are some:
- Food
- Activity
- Stress
- Excitement
- Heat
- Cold
- Types of foods consumed
- Growth spurts
- Sleep
- Illness
- What color pants she’s wearing (Just kidding about this one, but sometimes I wonder!)
We keep really good records of Mackenna’s BG numbers, amount of carbs consumed, amount of insulin delivered. We use a continuous glucose monitor to get a glimpse at what her BG levels are doing between finger pokes. And when we notice a pattern that recurs three days in a row, we make a small dose change to try and fix it.
Lately I’ve been kind of fed up with diabetes. A few weeks ago we battled all-day-long low blood sugars. So I made a tiny dose adjustment to keep her in a safer range, especially at school. The following week we had the opposite problem. High BGs all day. Another tiny adjustment. And this week we’ve been all over the board. Low all night long and high all day at school.
There was one night recently that had me giving her carbs every few hours at night to get her low BG up. Around 3am, she was in the low 100s and I felt safe letting her (and me) sleep through until morning. Well, morning came quickly when our 2-year-old was climbing in bed with us at 5:30am, telling us that he was awake. I rolled over to check the glucose monitor screen on my nightstand and saw that Mackenna had climbed up to the mid-200s in the 2 1/2 hours since I last checked her. So. Frustrating! Exhausted and discouraged, I complained to my husband, “I am doing everything right and it’s all just a crapshoot!” To which my sweet 2-year-old replied, “Crapshoot?” New word for him! Oops! We got a good laugh out of his tiny, chipper toddler voice saying that very adult word. A little comic relief in the middle of a frustrating moment.
Unsure whether or not it was actually a word, I looked “crapshoot” up in the dictionary. Oh, it’s a real word. Unpredictable? Risky? Gamble? That basically sums up what it’s like trying to be a pancreas. But it’s a risk I’ll take again and again. Because when she’s 14 or 16 or 18 and wants to manage her diabetes independently, I want to be able to look her in the eye and let her know that I have done the best I possibly could. And I want her to see my vigilance and persistence and mirror it as she starts to take the responsibilities on herself.
One number at a time. Treat it. Correct it. Learn from it. Move on from it.
We need a cure. Because no one is as good as a pancreas.
.PNG)


